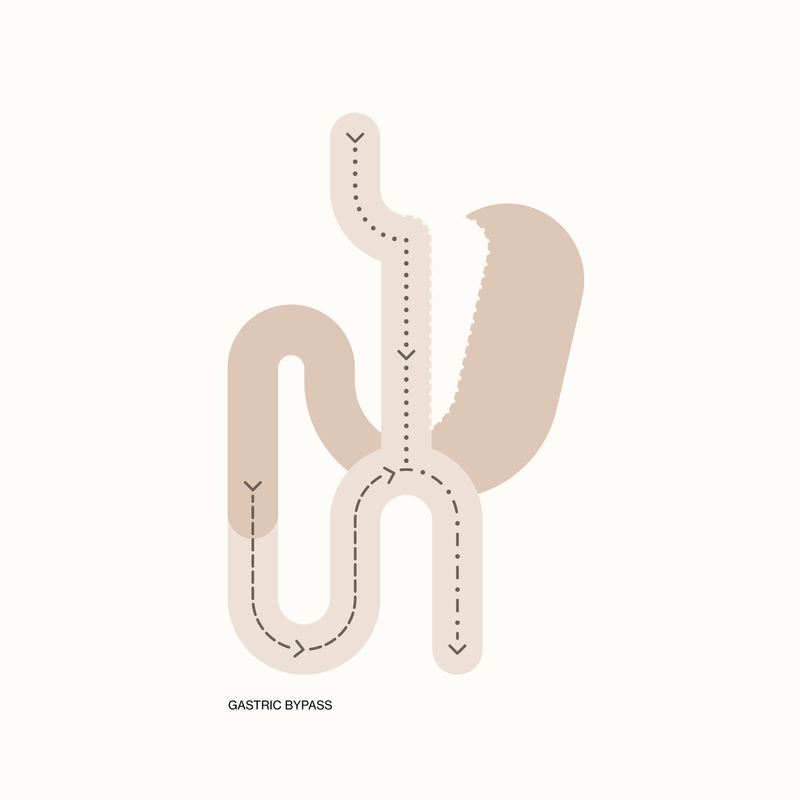
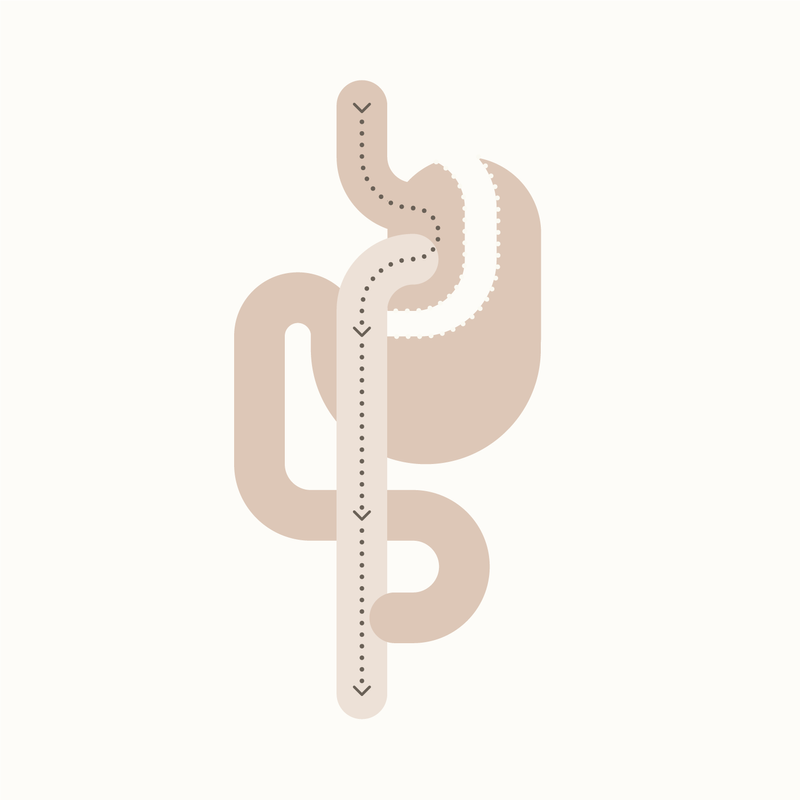
Dr Balalis offers two types of Gastric Bypass surgery – one anastomosis and Roux-en-Y.
‘One anastomosis gastric bypass’ refers to there only being one join between the stomach and the small bowel. This is compared to a Roux-en-Y gastric bypass, which has an added join between two parts of small bowel.
EXPLORE ONE ANASTOMOSIS GASTRIC BYPASS
EXPLORE ROUX-EN-Y GASTRIC BYPASS
If you’d like to discuss Gastric Bypass surgery or other surgical and non-surgical weight loss options, contact us anytime to schedule an appointment with a member of the team.